The term arthritis is defined as acute or chronic joint inflammation. Although there are many types of arthritis, including rheumatoid arthritis and psoriatic arthritis, osteoarthritis in the most common form. Osteoarthritis affects millions of active and sedentary adults worldwide.
Osteoarthritis involves changes in a joint’s cartilage and bone that may lead to joint pain and swelling. Osteoarthritis typically affects the joints of the knees, hips, lower back, neck, and small joints of fingers, thumb, and big toe. Pain associated with osteoarthritis is typically described as an aching or burning joint pain that gets worse with activity. The affected joint will often feel stiff and painful in the morning for about an hour and then feel sore again towards the end of the day.
WHAT CAUSES ARTHRITIS?
A healthy joint will have solid layers of articular cartilage that allow smooth movement and force absorption between bones. These layers of cartilage are maintained by cells called chondrocytes. In an arthritic joint there is a shift in the chondrocyte activity leading to decreased cartilage production and impaired cartilage maintenance.
This change in chondrocyte activity causes an increase in immune cell activity which can result in inflammation in the joint, with subsequent pain. Altered chondrocyte activity may be due to age, inflammation, joint injury, mechanical load and obesity, and genetics.
COMMON MISBELIEFS ABOUT ARTHRITIS
“Exercise will damage my joints more by increasing the force between the bones.”
Decreasing or stopping regular exercise due to osteoarthritis can lead to reduced muscle strength around the joint, decreased flexibility, weight gain, and difficulty with normal daily activities. Strengthening and stretching the muscles around an arthritic joint can actually decrease the friction and load on the joint. Regular exercise can keep the muscles around the joint strong, decrease bone loss, and can help control joint swelling and pain. Movement of joints also promotes the production of synovial fluid, which acts as a lubricant to reduce joint friction. It is well documented in research literature that regular participation in an appropriate exercise program can increase joint motion and strength, increase aerobic capacity, and improve physical and psychological function in people with osteoarthritis.
“Arthritis is degenerative, so my pain and function are only going to get worse as I age”
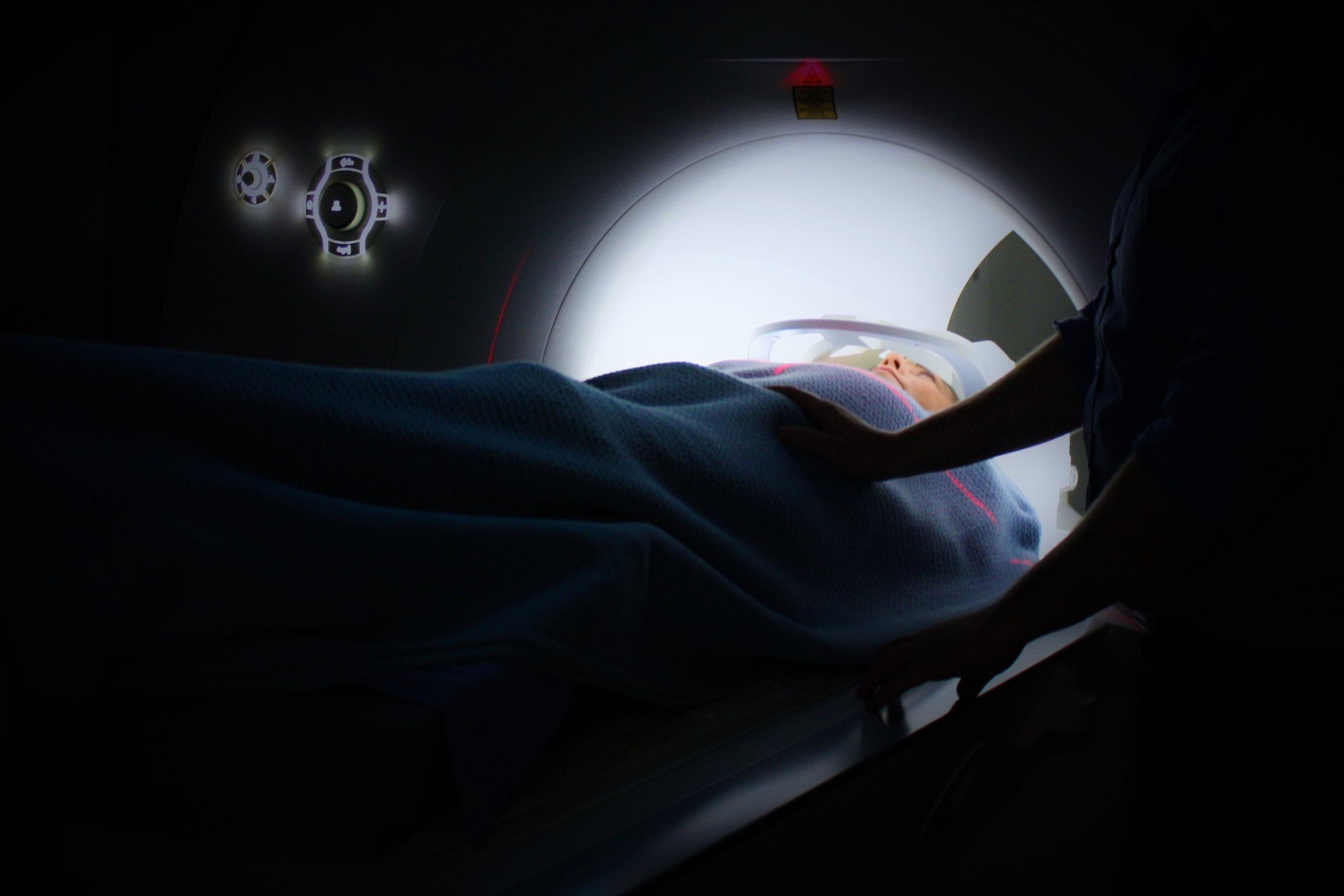
As we age, osteoarthritic changes may become more pronounced on imaging, including x-rays and MRI. However, your strength, function, and pain do not have to worsen just because a joint is becoming more arthritic. Many people get concerned when they are told their x-rays are positive for osteoarthritis or signs of degeneration. However, even though your joint may look a certain way on imaging it does not mean you will have pain or difficulty using that joint in daily and higher level activities.
“I have arthritis in my knees so I should only be doing low impact activities, like swimming and biking”
Low impact exercises like swimming, biking, and elliptical machines can be great aerobic activities for people with osteoarthritis, especially if they are beginning an exercise program or have limited mobility due to their osteoarthritis. However, these exercises should be part of a program that also incorporates mobility and strengthening exercises. A good exercise program involves finding the right type of exercises that allow you to keep moving without high levels of pain. If swimming and biking help accomplish this, then it is perfectly fine to make these a staple of the program. However, if you have a goal to walk with less pain, walking eventually needs to be a part of your program, with graded progressions in time or distance when appropriate.
“Running causes arthritis and will ruin your knees in the long-term”
Many of the long-term studies on runners suggest that, as long as your knees are healthy to begin with, running does not increase the risk of developing arthritis, even if you run into middle age or beyond. In some studies, runners show less overall risk of developing arthritis compared to less active individuals. Other studies have even suggested that regular loading of cartilage with appropriate rest periods may help encourage cartilage cells to divide and improve cartilage health in the long-term.
IN SUMMARY: KEEP MOVING, STAY STRONG, AND FIND THE RIGHT PROGRAM FOR YOU!
Osteoarthitis can be painful and lead to impaired mobility and activity. However, finding the right combination of activities, improving your strength and flexibility, and staying consistent over time can result in decreased pain and improved function. Remember that you are not your x-ray and pain-free activity may be possible despite what the imaging shows. It may take time and work, but the right aerobic, strength, and flexibility program can go a long way in combating osteoarthritis pain.